What is an implantable cardioverter-defibrillator (ICD) and how can it help?
The natural course of heart failure has one of two endings. An individual can eventually die from a problem called pump failure, when the heart becomes so weak that it no longer pumps. The other frequent scenario is sudden cardiac death due to an erratic or wildly fast heartbeat in the ventricle, with ineffective heart contractions. Once this abnormal rhythm takes hold, the only way to correct it is by administering a jolt of electricity to the heart muscle to shock it back into a normal rhythm. Only five in 100 people who have one of these episodes survive long enough to get to the hospital.
Heart arrhythmias are prevalent among people with heart failure. Heart muscle damage, especially following a heart attack, can interfere with the electrical conduction pathways through the muscle. The problem is compounded by the fact that most of the drugs routinely used to stabilize irregular rhythms also diminish the force of the hearts contractions, an incompatible side effect for people whose hearts are already weak.
In the 1980s, doctors tested a revolutionary concept-a miniature device implanted into the chest that would sense an abnormal rhythm and immediately deliver an electric shock (see Figure 10, above). This was the first implantable cardioverter-defibrillator (ICD). Since then, the units have become smaller, more complex, and more power-efficient, leading to their widespread use.
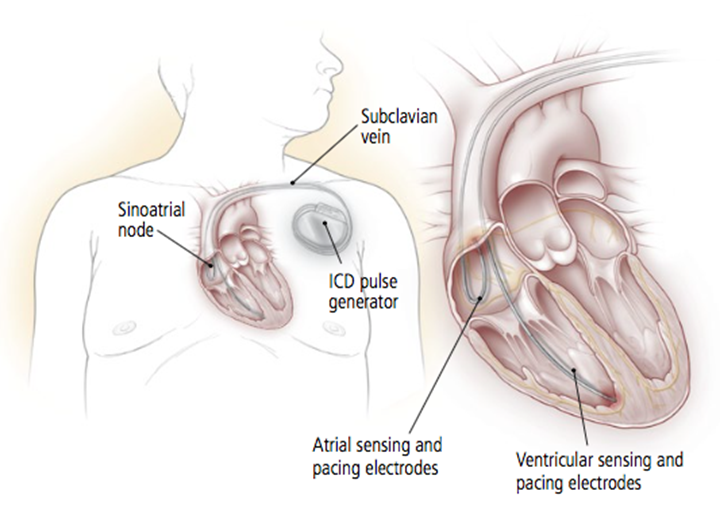
An implantable cardioverter-defibrillator (ICD) detects abnormal, potentially deadly heart rhythms and automatically corrects the faulty rhythm. For the insertion, which is done under local anesthesia, the surgeon places electrodes in the patients heart through one of the large veins in the chest and tests them. Then a small generator is placed under the skin in the chest. If and when this device senses an abnormal rhythm, the ICD restores the hearts normal beat, either by delivering a shock to the heart muscle or by using repeated low-energy signals (cardiac pacing). The device also records when abnormal rhythms occur and when shocks are administered. |
Many clinical trials have evaluated how ICDs stand up against traditional drug therapy in a variety of populations. One noteworthy trial assessed the performance of ICDs in people who had experienced a heart attack and had a low left ventricle ejection fraction-a marker for heart failure. The death rate among people assigned to the ICD group was 31% lower than in the group receiving drug therapy. This outcome was so overwhelmingly positive that investigators halted the study early. In addition, participants in both groups were receiving optimum drug therapy for heart failure, showing that the ICD produced benefits over and above those derived from drugs.
Most of the time an ICD works in the background, completely unnoticed. It silently and automatically monitors heart rate and rhythm. But when it detects a potentially deadly arrhythmia and delivers a jolt of electricity to halt it, the person notices. The jolt has been described as feeling like a kick in the chest.


